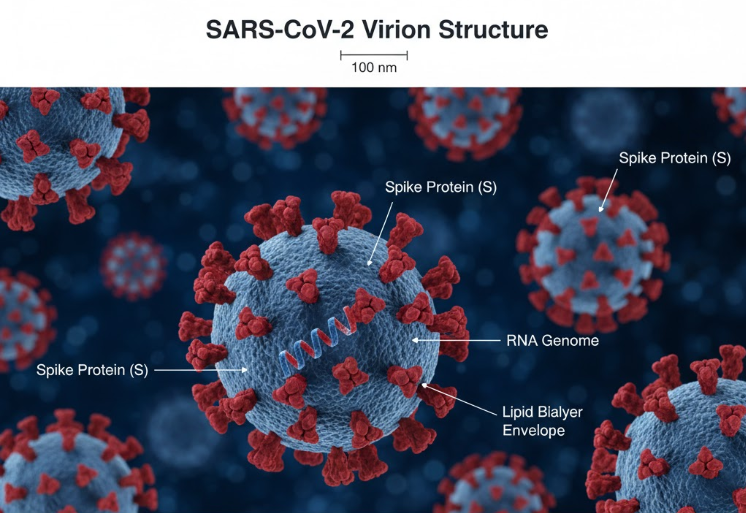
When scientists first identified the SARS-CoV-2 virus in late 2019, few could predict how quickly it would evolve. Over the next few years, the virus mutated into multiple variants, each changing the course of the pandemic. These mutations influenced infection rates, vaccine strategies, and global public-health responses. Understanding how and why these variants emerged is key to preparing for future outbreaks.
What Are Variants and Mutations?

All viruses mutate — it’s part of their survival strategy. A mutation occurs when the virus replicates and makes tiny copying errors in its genetic material. Most changes are harmless, but some can give the virus advantages such as:
- Higher transmissibility
- Ability to evade immunity
- Altered disease severity
When a set of significant mutations occurs, forming a genetically distinct version of the virus, it’s classified as a variant.
The World Health Organization (WHO) designates variants as:
- Variants of Interest (VOIs) — under observation for potential risk.
- Variants of Concern (VOCs) — confirmed to have increased transmissibility, virulence, or immune escape potential.
Major COVID-19 Variants and Their Global Impact
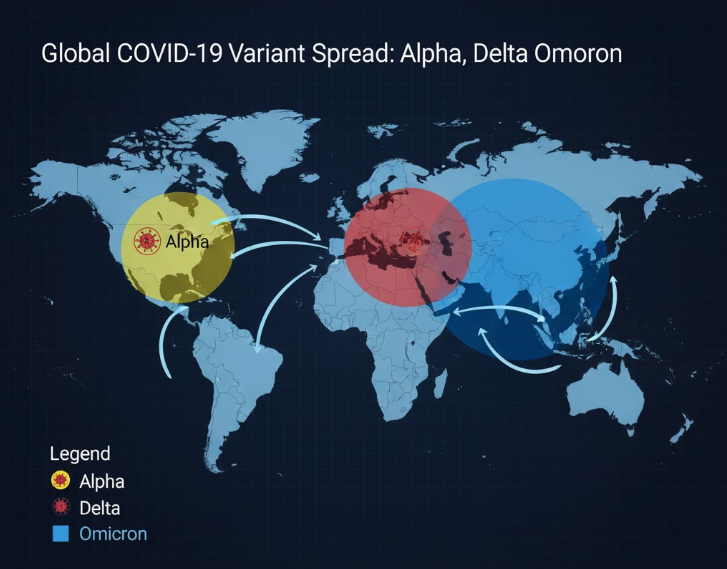
1. Alpha (B.1.1.7) — The UK Variant
- First detected: September 2020 in the United Kingdom.
- Key mutations: N501Y (increased binding to human cells).
- Impact: Around late 2020–early 2021, Alpha became the dominant strain across Europe and North America, causing sharp spikes in cases.
- Effect: Estimated to be 40–70% more transmissible than the original strain, leading to stricter lockdowns in the UK and many other countries.
2. Beta (B.1.351) — The South African Variant
- First detected: December 2020 in South Africa.
- Key mutations: E484K and K417N (helped the virus escape antibodies).
- Impact: Raised concerns about vaccine effectiveness, as early studies showed reduced neutralization by antibodies from Pfizer and AstraZeneca vaccines.
- Global response: WHO and vaccine developers began adapting vaccine formulations and monitoring breakthrough infections.
3. Gamma (P.1) — The Brazilian Variant
- First detected: November 2020 in Manaus, Brazil.
- Key feature: Reinfections became more common, even among those who had recovered from earlier strains.
- Effect: Overwhelmed Brazil’s healthcare system and spread to several countries in South America, illustrating the risk of uncontrolled transmission leading to new mutations.
4. Delta (B.1.617.2) — The Indian Variant
- First detected: October 2020 in India.
- Key mutations: L452R and P681R (enhanced infectivity).
- Impact: Delta became the most dominant global strain in mid-2021, driving severe waves of infection across India, Southeast Asia, and the U.S.
- Effect:
- Up to 2x more transmissible than Alpha.
- Led to catastrophic surges in hospitalizations and deaths in India’s second wave (April–May 2021).
- Vaccines still worked but were less effective at preventing infection, emphasizing the importance of booster doses.
5. Omicron (B.1.1.529) — The Global Game-Changer
- First detected: November 2021 in South Africa and Botswana.
- Key features: Over 30 mutations on the spike protein — an unprecedented number.
- Impact:
- Spread globally within weeks, replacing Delta by early 2022.
- Highly transmissible but generally caused milder disease in vaccinated populations.
- Sub-variants (BA.1, BA.2, BA.4, BA.5, XBB, etc.) kept evolving through 2022–2023, each with slight immune-escape advantages.
- Effect:
- Triggered record case numbers but fewer deaths due to vaccination and prior immunity.
- Pushed vaccine makers (like Pfizer and Moderna) to release updated “bivalent” boosters targeting Omicron.
How Variants Affected Vaccines and Treatments
Each new variant tested the limits of medical science:
- Vaccine adaptation: While original vaccines continued preventing severe illness, Omicron’s mutations reduced protection against mild infections. Booster campaigns became essential to maintain immunity.
- Monoclonal antibody resistance: Some treatments lost effectiveness as variants evolved, forcing continuous revision of therapeutic recommendations.
- Diagnostic adjustments: PCR and antigen test kits were updated to detect emerging strains without false negatives.
Global Lessons Learned

1. Genomic Surveillance Matters
Countries with robust sequencing programs (like the UK, India, and South Africa) detected variants early, giving the world time to respond. WHO’s Global Initiative on Sharing All Influenza Data (GISAID) became a vital hub for tracking viral evolution.
2. Vaccine Equity is Crucial
Unequal access to vaccines allowed uncontrolled spread in low-income nations — creating the ideal conditions for new variants to emerge.
As WHO stated, “No one is safe until everyone is safe.”
3. Preparedness Must Be Continuous
The pandemic showed that variant evolution doesn’t stop when cases decline. Continuous research, surveillance, and vaccine updates are essential for future health security.
Conclusion
COVID-19 variants reshaped the pandemic’s trajectory — from the deadly waves of Delta to the widespread yet milder Omicron surge. Each mutation taught the world more about viral behavior, vaccine adaptation, and the interconnectedness of global health.
Though the WHO declared in 2023 that COVID-19 was no longer a global public health emergency, variants continue to circulate. The experience reminds us that science, vigilance, and solidarity are the strongest tools against an ever-changing virus.