The global response to the COVID‑19 pandemic has revolved around two key pillars: prevention via vaccination and medical treatment of infection. While vaccines aim to stop illness before it starts, treatments target those who fall ill despite preventive efforts. Yet, despite scientific advances, vaccine hesitancy and unequal access to treatments continue to challenge public-health efforts worldwide. This article explains how COVID-19 vaccines work, what treatments are now recommended, and explores the main reasons behind hesitancy.
How COVID-19 Vaccines Work

The immune system and vaccination
A vaccine mimics an infection so your body’s defences can recognise and fight the real germ later. According to the World Health Organization (WHO), when you receive a vaccine your immune system is exposed to an antigen (or blueprint for one) which triggers antibody production and memory cell formation — so that when the actual pathogen appears, your body responds faster and more effectively. (World Health Organization)
Types of COVID-19 vaccines
There are multiple vaccine technologies. Some of the main ones include:
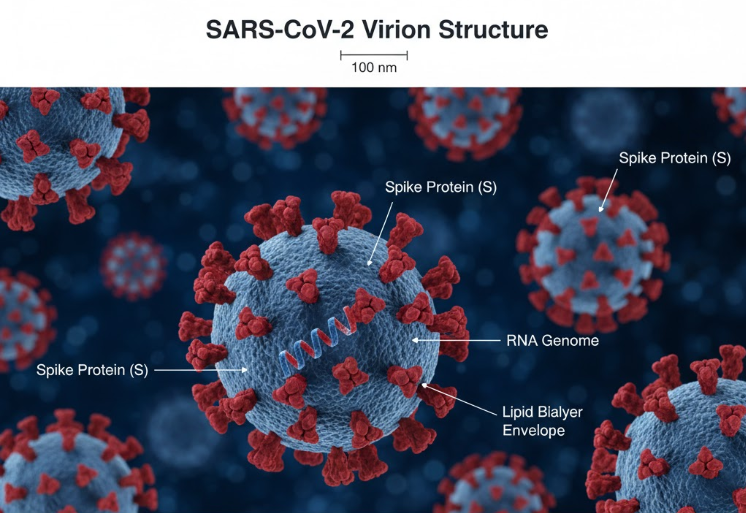
- mRNA vaccines – these carry messenger RNA instructions to your cells so they make a harmless piece of the virus (e.g., the spike protein) which then triggers the immune response. (CDC)
- Viral vector vaccines – these use a benign virus to deliver genetic instructions to produce the antigen. (World Health Organization)
- Protein subunit vaccines – these deliver purified parts of the virus (such as spike protein fragments) rather than genetic material. (Mayo Clinic)
Why multiple doses / booster shots

For some vaccines, your immune system needs a “primer” dose followed by a “booster” to build stronger and longer-lasting immunity. WHO notes that for COVID-19 several vaccines require two doses (or more) to reach their full protective potential. (World Health Organization)
What vaccines protect against
COVID-19 vaccines primarily aim to:
- reduce the risk of severe illness, hospitalisation and death, more than completely preventing any infection;
- contribute to population immunity, reducing virus spread when many people are immunised. (World Health Organization)
Treatments for COVID-19: What Works
Different therapeutic approaches
Once infection occurs, treatments for COVID-19 fall into several categories: antiviral medications (which target the virus itself), immune-modulators (which calm harmful inflammation), and monoclonal antibodies (lab-made antibodies that block the virus) among others. (U.S. Food and Drug Administration)
WHO-recommended treatments
According to WHO guidelines:
- The oral antiviral combination Nirmatrelvir + Ritonavir (sold as Paxlovid) is strongly recommended for people with non-severe COVID-19 who are at high risk of progression to severe disease. (World Health Organization)
- The drug Baricitinib (a JAK-inhibitor) is recommended for patients with severe or critical disease, in combination with corticosteroids. (World Health Organization)
- Monoclonal antibodies such as Sotrovimab and the combination Casirivimab + Imdevimab are conditionally recommended in specific cases. (World Health Organization)
Timing matters
Many treatments are most effective when administered early in the course of infection, before the disease becomes critical. Delayed treatment can reduce their benefit. (CDC)
Limitations and access challenges
Even though treatments exist, WHO emphasises the need for equitable access, affordable pricing, and ensuring low- and middle-income countries can obtain them. (World Health Organization)
Why Some People Hesitate: Vaccine Hesitancy & Treatment Uptake

What is vaccine hesitancy?
The WHO defines vaccine hesitancy as a “delay in acceptance or refusal of vaccination despite availability of vaccination services.” Several large-scale reviews show it is a serious barrier to achieving wide immunisation. (Frontiers)
Common reasons for hesitancy
Factors contributing to hesitancy include:
- Safety concerns and fear of side-effects (especially for new vaccines). (EMRO)
- Doubts about vaccine effectiveness, particularly if people perceive COVID-19 risk as low. (Frontiers)
- Speed of vaccine development causing mistrust (why was it produced so fast?). (Frontiers)
- Misinformation and conflicting messages, especially via social media. (Frontiers)
- Access and convenience issues, especially in low-resource settings (logistics, appointment systems, transportation). (PubMed)
Treatment uptake hesitation
Similarly, hesitancy or access issues for treatments can stem from:
- Lack of awareness of available therapies;
- Concerns over cost or availability;
- Delay in seeking care or diagnosis which reduces treatment effectiveness;
- Mistrust in healthcare or pharmaceutical systems.
Why It Matters
- Vaccines reduce the burden on healthcare systems, lower death rates, and enable societies to open up safely.
- Effective treatments reduce the severity of illness, shorten hospital stays, and give another layer of protection beyond prevention.
- High vaccine uptake and timely treatment uptake are essential for controlling the pandemic, especially as new virus variants emerge.
- Understanding hesitancy helps tailor communication, improve trust, and ensure equitable access globally.
Conclusion
Vaccination and treatment form a dual strategy: preventing infection and mitigating disease when it occurs. The science behind how vaccines and treatments work is robust, and global health authorities, including WHO, have provided clear guidance. Yet science alone isn’t enough — public trust, access, equity and clear communication are equally vital. Overcoming hesitancy and ensuring all communities benefit from these breakthroughs remains one of the major global health tasks of our time.